Beta hCG Levels After IVF Embryo Transfer
Medically reviewed by Linda Streety, RN, BSN
Human chorionic gonadotropin (hCG), sometimes referred to as the “pregnancy hormone,” is a hormone produced by cells in the placenta. The hCG hormone stimulates the corpus luteum, a completely normal cyst that forms from the follicle after ovulation, to produce progesterone. Progesterone plays an important role in maintaining pregnancy through its early stages by thickening the uterine lining, modulating immune system response so it doesn’t reject the fetus, and preventing uterine contractions (1). HCG levels rise rapidly in your blood for the first two months of a pregnancy, fall quickly in the third month, then stabilize at a lower level until delivery.
As the amount of hCG in your blood increases in the early weeks of pregnancy, it can be detected by a beta hCG blood test. This test is one of the best ways to identify an early pregnancy and monitor its growth. Since the rate at which hCG is increasing is more important than the overall amount, your clinician may order hCG pregnancy tests two days apart (also known as a serial hCG blood test), which will give them valuable information about how your pregnancy is progressing.
What are good IVF hCG levels after embryo transfer?
After embryo transfer, it takes a few days for an embryo to implant in your uterine lining and connect to the blood vessels that will support its growth. Only then can hCG begin to rise enough to be detected!
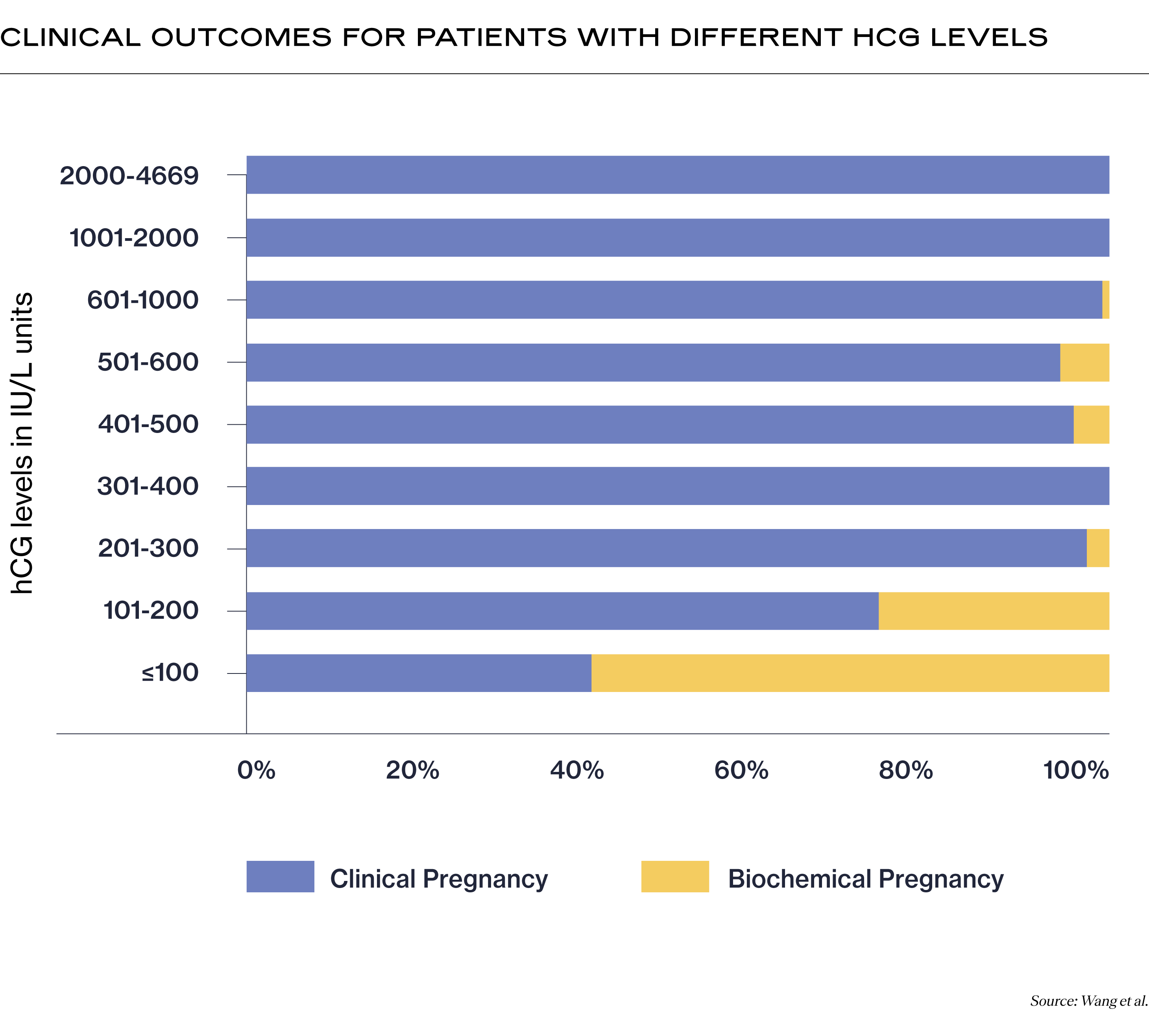
Below are the results of a study of 523 pregnancies looking at the relationship between hCG levels and pregnancy outcomes after IVF. It used both fresh and frozen transfers and measured hCG levels 14 days after day 3 embryo transfers, and hCG levels 12 days after day 5 embryo transfers (2).
It may help to know what each of the terms below mean, first:
-
A clinical pregnancy occurs when a positive hCG pregnancy test is followed by an ultrasound that confirms a pregnancy in the uterus, either by spotting the gestational sac (the cavity of fluid surrounding the fetus in its early weeks) or hearing a fetal heartbeat.
-
A biochemical pregnancy is a very early stage miscarriage that occurs within the first 5 weeks of pregnancy. While the implanted embryo produced enough hCG to show up on an hCG test, it will stop developing and hCG levels will fall.
With that said, here is a chart of hCG levels after embryo transfer:
If you have a clinical pregnancy, your hCG may then indicate issues with your pregnancy, such as an early pregnancy loss or ectopic pregnancy. Again, it may be helpful to know what the terms mean, first:
-
Ongoing pregnancy is defined as a viable pregnancy that reaches 12 weeks gestation.
-
Early pregnancy loss occurs when the pregnancy ends within the first 13 weeks of pregnancy. It is also referred to sometimes as a “miscarriage” or “spontaneous abortion.”
-
Ectopic pregnancy occurs when the embryo implants outside of the uterus, usually in the fallopian tube. Ectopic pregnancies are not viable and can be dangerous, so your clinician will take it seriously if they suspect one has occurred.
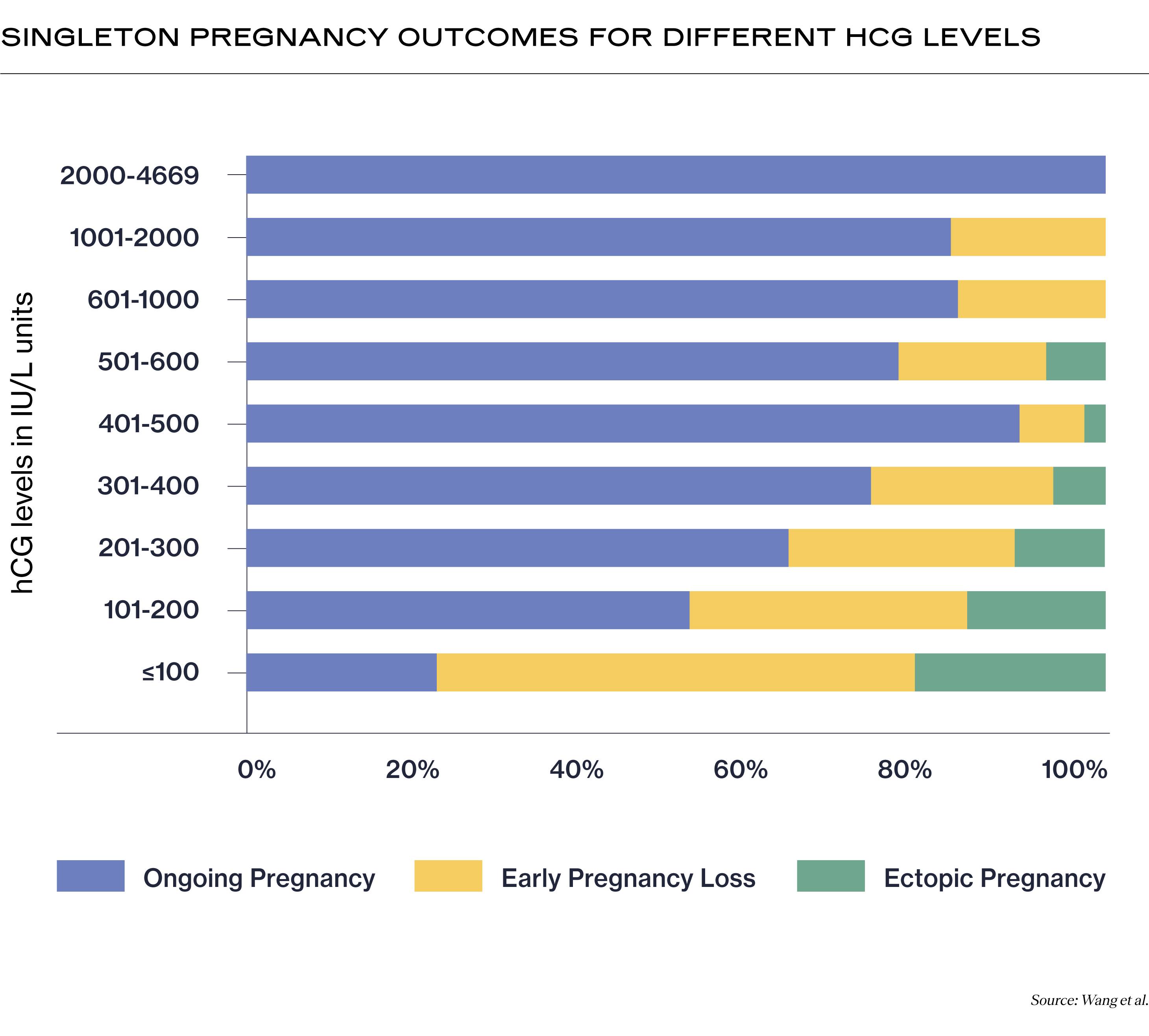
In this IVF hCG levels chart, we only included the hCG levels for a singleton pregnancy because pregnancy with multiples can get complicated depending on how many fetuses you are carrying, and since each fetus can have a different outcome.
These numbers give only a very partial picture of what may happen with your pregnancy. Your clinician will also be looking at the rate at which hCG is increasing in your blood. One study found that, on average, singleton IVF pregnancies that led to a live birth showed a relative hCG increase of 50% in one day and 124% in two days (3). By comparing hCG tests several days apart, your clinician will better understand whether your pregnancy is progressing on track.
What does it mean if my hCG isn’t increasing?
If your hCG levels are dropping, plateauing, or rising very slowly, that may indicate to your clinician that you are:
At risk of a miscarriage
When hCG levels are not progressing as they should, this can indicate that a miscarriage may occur (4).
Experiencing a biochemical pregnancy
Also known as a “chemical” pregnancy, this occurs when a miscarriage occurs very early in the pregnancy. These often occur because of chromosomal issues with the embryo.
Having an ectopic pregnancy
An ectopic pregnancy occurs when the embryo implants outside of the uterus. If your hCG levels are not rising as expected, your clinician may order an ultrasound to check your uterus for a gestational sac. Sadly, ectopic pregnancies are not viable and need to be removed from your body to prevent life-threatening complications. Your clinician can help determine how to best proceed, whether through medication or surgery. It may help to know that many people who experience an ectopic pregnancy go on to have a healthy pregnancy.
What does a high hCG level mean?
A high hCG level may mean that:
You are pregnant with multiples
HCG levels for twins, triplets, and other multiple pregnancies are higher because there are more embryos to produce hCG! One study found that after embryo transfer, hCG levels above 600 IU/l had a high chance of being a multiple pregnancy (6).
You have a molar pregnancy
A molar pregnancy occurs when the trophoblast cells that form the placenta grow abnormally. Sadly, molar pregnancies are not viable. This is because in a molar pregnancy with high hCG levels, there is no fetus, only placental cells (7).
You are carrying a fetus with Down syndrome
If your hCG levels are elevated, there’s a small chance that your fetus has Down syndrome (8), which is caused by an extra chromosome in the fetus’ cells. There are additional tests you can do if this is a concern. Your clinician may be able to detect fetal abnormalities on an ultrasound. You may also choose to have Down syndrome screening tests conducted after the 11th week of pregnancy.
What does a low hCG level mean?
If your levels of hCG are low but increasing steadily, it may indicate a miscarriage. However, healthy, ongoing pregnancies have occurred even with very low hCG levels on day 14 after embryo transfer. Consulting with your clinician can help you understand what is happening in your particular pregnancy.
HCG is not the only way to understand your pregnancy
While hCG is one of the first and best ways to detect the earliest stages of a pregnancy, your hCG level alone only tells your clinician a limited amount. Your clinician may order a serial hCG blood test or conduct an ultrasound to better understand the location and progression of your pregnancy and help you understand what is happening in your body. If you are concerned about your hCG level, you should talk with your clinician, who can help put your hCG level in context and offer next steps.
Recent Articles
References
-
Dante, G., Vaccaro, V., & Facchinetti, F. (2013). Use of progestagens during early pregnancy. Facts, Views & Vision in ObGyn, 5(1), 66–71. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3987350/
-
Wang, Z., Gao, Y., Zhang, D., Li, Y., Luo, L., & Xu, Y. (2020). Predictive value of serum β-human chorionic gonadotropin for early pregnancy outcomes. Archives of Gynecology and Obstetrics, 301(1), 295–302. https://doi.org/10.1007/s00404-019-05388-2
-
Chung, K., Sammel, M. D., Christos Coutifaris, Raffi Chalian, Lin, K., Castelbaum, A. J., Freedman, M. F., & Barnhart, K. T. (2006). Defining the rise of serum HCG in viable pregnancies achieved through use of IVF. Human Reproduction, 21(3), 823–828. https://doi.org/10.1093/humrep/dei389
-
Letterie, G. S., & Hibbert, M. (2000). Serial serum human chorionic gonadotropin (hCG) levels in ectopic pregnancy and first trimester miscarriage. Archives of Gynecology and Obstetrics, 263(4), 168–169. https://doi.org/10.1007/s004040050275
-
Lozeau, A.-M., & Potter, B. (2005). Diagnosis and Management of Ectopic Pregnancy. American Family Physician, 72(9), 1707–1714. https://www.aafp.org/pubs/afp/issues/2005/1101/p1707.html?utm_medium=email&utm_source=transaction
-
Guth, B., Hudelson, J., Higbie, J., Solomon, B., Polley, S., Thomas, S., & Gentry, W. L. (1995). Predictive value of hCG level 14 days after embryo transfer. Journal of Assisted Reproduction and Genetics, 12(1), 13–14. https://doi.org/10.1007/BF02214122
-
Goldstein, D. P., & Berkowitz, R. S. (1994). Current management of complete and partial molar pregnancy. The Journal of Reproductive Medicine, 39(3), 139–146. https://europepmc.org/article/med/8035368
-
Banerjee, S., Smallwood, A., Chambers, A. E., Papageorghiou, A., Loosfelt, H., Spencer, K., Campbell, S., & Nicolaides, K. (2005). A link between high serum levels of human chorionic gonadotrophin and chorionic expression of its mature functional receptor (LHCGR) in Down’s syndrome pregnancies. Reproductive Biology and Endocrinology, 3(1), 25. https://doi.org/10.1186/1477-7827-3-25
Share this
Recent Articles
Learn everything you need to know about IVF
Join the newsletter for IVF education, updates on new research, and early access to Alife products.